News Items
- 05-Feb-2012
"ALSG approved Safe Transfer & Retrieval (STaR) course, Belfast - November 08th & 09th 2012" - 09-Oct-2011
"Survival-linX Solutions on-line Classrom & Education Centre" - 24-Sep-2011
"RIDDOR - Changes to incident reporting" - 12-Mar-2011
"Do you know what to do if a child is choking?" - 12-Mar-2011
"Anaphylaxis - recognition and management" - 12-Mar-2011
"Join use on Facebook - for all the latest discusions, first aid advice and general resuscitation information" - 12-Mar-2011
"Does your Surgery need Life Support (CPR) & Automated Defibrillator (AED) Training?" - 12-Mar-2011
"Resuscitation Council (UK) Emergency Life Support in Schools" - 04-Nov-2010
"2010 Resuscitation Guidelines - Summary of main changes" - 07-Sep-2010
"Do you have a Automated Defibrillator in your place off work?" - 24-Nov-2009
"Survival-linX Solutions gains HSENI certificate of approval to provide first aid at work (FAW) training courses." - 07-Nov-2009
"Risks of pandemic H1N1 2009 influenza (swine influenza) during cardiopulmonary resuscitation (CPR)" - 19-Oct-2008
"Are you thinking of purchasing an Automated External Defibrillator(AED) - essential infomation to assist you when choosing the correct unit." - 09-Aug-2008
"An account of the formation of the foramen ovale and how blood entering the inferior vena cava receives preferential blood streaming in the foetus." - 31-Aug-2007
"Mechanical CPR - Lund University Cardiopulmonary Assist System (LUCAS)" - 02-Jun-2003
"Significant increase in training for Health Care professionals likely to be called to assist children with trachestomy tube difficulties"
Mechanical CPR - Lund University Cardiopulmonary Assist System (LUCAS)
31-Aug-2007
Victims of cardiac arrest require rapid and effective chest compressions for an optimal chance of successful defibrillation and to decrease the likihood of neurological deficit (Nolan et al 2005). Chest compressions by the rescuer artificially produce a blood flow by manually compressing the victim’s chest maintaining cerebral and coronary perfusion. Inadequately performed chest compressions might compromise patient survival (Van Hoeyweghen et al 1993) by producing insufficient blood flow required to maintain critical organ perfusion in particular perfusion to the brain leading to neurological damage. Hightower et al (1996) concluded that where manual chest compressions were performed quality declined significantly over a five minute period. These findings are supported by a number of other studies which concluded that rescuers can only perform effective compressions for a short period of time due to rescuer fatigue (Ashton et al 2002, Ochoa et al 1998).
Interruptions to chest compressions occurs commonly with one study concluding rescuers provided chest compressions less than half of the time that was required (Valenzuela et al 2005). A number of studies have also shown that prolonged manual chest compressions produce an insufficient blood flow and at best effective cardiopulmonary resuscitation (CPR) produces twenty to thirty percent of normal cardiac output (Woorhees et al 1980, Weil et al 1985, Rubertsson et al 1995). It is well documented that rescuer life support skills and performance varies. Moser and Coleman (1992) reported that although most people can learn CPR these skills begin to deteriorate in both laypeople and healthcare professionals as early as two weeks after initial training. In an effort to improve survival and quality of life for victims of cardiac arrest recent guidelines published by the Resuscitation Council (UK) placed greater emphasis on the rescuer performing effective cardiopulmonary resuscitation (CPR) by recommending the number of chest compressions are increased from fifteen to thirty per CPR cycle and that rescuers swap over every two minutes to avoid fatigue (Nolan et al 2005).
In recognition of the combined limitations with manual compressions several manual (non-automatic) and mechanical (automatic) compression devices have been developed for use in adult cardiac arrest. Lund University Cardiopulmonary Assist System (LUCAS) is one such automated resuscitator device which has become popular in Great Britain and Europe both in the hospital and in particular the prehospital sector (Halliwell 2005). The aim of this article is to assess the possible advantages and disadvantages of using LUCAS and the operational limitations that exist in its deployment for cardiac arrest victims.
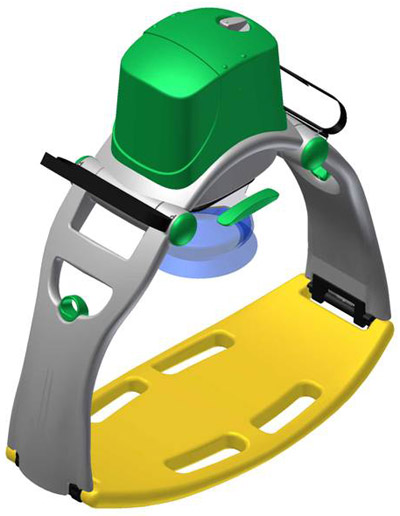
LUCAS – External Cardiac Compressor
LUCAS is an easy to carry portable device that can be applied to the patient in less than twenty seconds making it suitable for the patient either in or outside the hospital setting (Jolife, LUCAS instructions for use manual 2005). The device can be considered for use when the rescuer has confirmed cardiac arrest in the adult victim (>/= 16yrs old), providing there are no contraindications which are discussed later. LUCAS is a non invasive, gas driven light weight (6.5kg) cardiac compression device used to mechanically perform effective, consistent, uninterrupted automatic compression and active decompression of the patient’s chest. Once activated LUCAS delivers one hundred compressions/minute to a depth of 5cms. The total dedicated compression-decompression time (duty cycle) is divided equally between active compression and the active decompression (duty cycle of 50:50). LUCAS consists of two parts (appendix 1) an upper part consisting of a pneumatically driven piston rod which squeezes the patients sternum via a pressure pad which is surrounded with a suction cup to provide active decompression and a back plate to which the upper part is attached (Jolife, LUCAS instructions for use manual 2005). The device is powered by a continuous source of compressed gas either oxygen or air.
Contraindications/Restrictions
The manufacturers recommend that LUCAS is contraindicated in patients that are too small i.e. where the distance between the pressure pad and the patients sternum exceeds 15mm or in the large/obese patient i.e. where the support legs of the device cannot be locked onto the backboard due to patient sternal height (Jolife, LUCAS instructions for use manual, 2005). The device is not suitable for children and heavily pregnant women. Children require a much less depth of compression than LUCAS provides and heavily pregnant woman require a lateral tilt to avoid splinting of the diaphragm and compression of the abdominal aorta. The device is not recommended to operate with the patient in a lateral tilt therefore patients in the third trimester of pregnancy are also classified as a contraindication for LUCAS use. One case report by Vatsgar et al (2005) however reported successful resuscitation with no complications of a lady who was 24 weeks pregnant following manual and then LUCAS CPR.
Concerns have been raised regarding the risk of fire due to the high atmospheric oxygen concentration generated as a result of LUCAS exhaust gases when powered with an oxygen gas source. The potential risk of injury due to an oxygen enriched atmosphere was first highlighted by a safety notice issued by the Medical Devices Agency (1995) which recommended that users of defibrillators should ensure there is no increase in oxygen concentration around the patient head and upper body. Farmery and Carter (2007) concluded that oxygen concentrations when using LUCAS in the cabin of a helicopter rose no higher than 23% and that LUCAS was a safe device to use during transfer. Critical review of this paper revealed that the oxygen analysers used to assess atmospheric oxygen were a significant distance (1 metre) from the LUCAS device, concentrations were not analysed around the area where defibrillation pads are applied(patient chest) and where the danger of explosion is highest due to defibrillation sparking. A more recent paper by Deakin et al (2007) measured peak atmospheric oxygen concentrations over a manikin chest of 36.7% in a resuscitation bay in the hospital setting. In a ventilated ambulance this study recorded peak atmospheric oxygen concentration at 33.8%. Deakin et al (2007) concluded that it was likely that the use of LUCAS when powered by oxygen during resuscitation risked fire or explosion if defibrillation was required.
Automatic mechanical vs. manual compressions
Advantages
In comparison with manual CPR, mechanical devices such as LUCAS adheres to the guidelines at all times and maintain CPR qualitatively close to 100% (Sunde et al 1997). Consistent, sustained high quality chest compressions are delivered at a rate of 100/minute and to a depth of 4-5cms. This achievement meets the statistical requirements to achieve cardiac compressions proposed by the Resuscitation Council UK (Lockley et al 2001) who recommend effective CPR should be a sufficient number of chest compressions per minute (between 80 – 100), and sufficient depression of the sternum to ensure compression of the heart (4 – 5 cms in adults). The chief advantages of mechanical devices are longevity – they can keep operating providing the power source does not run out and quality does not vary over time.
Most mechanical compression devices have been marketed on the clinical benefits they provide to the patient and have not considered the benefits to the rescuer (Lafuente and Melero-Bascones 2004). CPR is often performed in a compromised working position or in circumstances that prevent bed height adjustment to between knee and mid-thigh of the rescuer with their feet shoulder width apart as per safe handling recommendations (Resuscitation Council (UK) 2001). CPR requires forward and backward movement of the rescuer trunk an action that if incorrectly performed or if repeated for a long period results in muscle fatigue introducing stress on the spine and inevitable back injury (Jones 2004). These actions combined with unsafe positioning may increase the likelihood of rescuer lower back injury. Jones (2004) reported findings which concluded that 90% of nurses complained of back discomfort during or after performing CPR with a further 40% of nurses claiming back injury was directly related to the CPR procedure. These statistics support the need for both safe positioning of the rescuer and reduction in prolonged periods of CPR. This need can be delivered by LUCAS and other mechanical devices which replace manual compressions thus preventing injury.
Mechanical CPR frees the rescuer(s) to undertake other life saving procedures and treatments. This is an advantage for all healthcare professionals attending a cardiac arrest however this factor is clearly immense for the prehospital professional where manpower resources are limited and transportation of the patient requiring CPR is sometimes required. The ability to use this device safely and effectively during transportation is a great advantage to prehospital healthcare personnel. In a moving ambulance it is impossible to deliver adequate chest compressions (Stapleton 1991) and any attempts at performing CPR would inevitability put ambulance staff at considerable risk of injury as they would be unrestrained in the vehicle. LUCAS can be applied safely and effectively to the patient on the ground, on a bed or on a stretcher whether static or moving. Steen et al (2005) concluded that LUCAS was safe to use during transport after testing the device secured to a manikin in a moving ambulance which was crash tested at a speed of 30km/hr. Critical review of the Steen et al (2005) paper revealed funding had been received from the hospital that designed LUCAS, further independent research would be useful to validate their conclusion.
Manual CPR involves two important phases both which are equally important, chest compression and decompression. Following compression the rescuer must allow passive recoil of the patient chest which requires an active release of downward pressure to allow the chest wall to recoil (decompression) and the heart to refill with blood. Aufderheide et al (2006) studied rescuers providing chest compressions and observed a high incidence of incomplete chest decompression. Yonnopoulos et al (2005) concluded that if the rescuer did not adequately allow for full chest decompression this led to a significant detrimental effect on coronary artery and cerebral perfusion pressure, impedes venous return compromising aortic pressures which has been associated with poor survival prognosis. LUCAS provides active decompression guaranteeing one hundred percent chest wall recoil which may optimize patient haemodynamics, organ perfusion and survival (Lurie et al 2001).
Compared with other active mechanical CPR devices LUCAS is light weight (6.5kg) and easy to transport to the scene of the cardiac arrest victim. Following a basic two hour training course a single rescuer can rapidly apply and operate LUCAS within twenty seconds to any patient regardless of size providing there are no contraindications.
Disadvantages - Traumatic complications
Cardiac compressions performed by either layperson or healthcare professional have been associated with a wide range of accidental patient injuries such as pulmonary haemorrhage, sternal and/or rib and liver injury reported. A comprehensive literature review of the incidence of patient sternal and rib fractures undertaken by Hoke and Chamberlain (2004) found that in cardiac arrest victims that received manual CPR, one fifth had sternal fractures and one third had rib fractures. These statistics are supported by similar finding in another study undertaken by Black et al (2004).
Baubin (1999) reported that active mechanical compression-decompression CPR significantly increased rib and sternal fractures however acknowledged limitations to their study. Hoke and Chamberlain (2004) found no evidence of an increased complication rate with active compression-decompression devices however recommended the need for systematic reports of complications. In a letter to the editor of a resuscitation journal Englund and Kongstad (2006) focused attention on the atypical tissue damage observed in victims that did not survive cardiac arrest after receiving active compression cardiopulmonary resuscitation with suggestion that this may be due to the prolonged and more vigorous compressions delivered by the LUCAS device.
A study to determine the frequency of thoracic injuries in particular sternal trauma in female cadavers (Oberladstaetter et al 2005) after one minute of LUCAS compressions is ongoing and remains unpublished. The findings of this study if significant should guide health professionals as to the potential risks with the LUCAS device. Skin damage in the form of suction cup marks has been reported on the sternum of patients (Vatsgar et al 2005).
Disadvantages - General
LUCAS is a pneumatic device fully powered by compressed gas either oxygen or air. In Ireland and the United Kingdom oxygen powered devices are used as ambulance services do not carry compressed bottles of air. In the hospital setting compressed air is only available in acute areas e.g. theatres, intensive care and respiratory wards. The manufacturers report a gas consumption of 70 litres/minute (LUCAS technical data sheet, 2005) however Deakin et al (2007) reported an oxygen consumption of 115 litres/minute. Axelsson et al (2006) also observed greater gas consumption than the manufacturer stated. High gas consumption in the prehospital environment where only bottled gases are available is of concern. Most ambulances carry two of the standard F size oxygen cylinder which holds 1360 litres (when full) providing an approximate gas supply to last twenty four minutes. Transport time may exceed this perhaps at time of traffic congestion or during longer patient transfers; additionally oxygen is also required to provide adequate oxygenation of the patient which would reduce oxygen availability time even further. Cylinders F size or larger are not easy to transport due to weight (17kg) which restricts the device to the ambulance setting only requiring manual compressions to be performed by the ambulance crew prior to loading the patient into the vehicle.
The noise level from LUCAS when operating is quite high, but still within United Kingdom statuary regulations (Control of noise at work regulations, 2005). Steen et al (2005) reported a noise level of 83-88 dB (A), same for dB (L) and a peak value of 111 dB when LUCAS was operational in a stationary ambulance with the vehicle engine running and suggested that if the noise is felt disturbing then ear plugs could be used. This suggestion would restrict communication amongst rescuers and therefore is not practical. In practice noise produced by LUCAS active compression-decompression is tolerable however as suggested by Axelsson et al (2006) noise level will hopefully be addressed in later revised models.
Mechanical CPR in special circumstances.
Resuscitation requires modification in special medical circumstances and in some cases prolonged resuscitation may be required (Soar et al 2005). For example it is recognised that in hypothermic patients prolonged CPR may need to be provided to allow rewarming before there is likelihood of a patient response. Over a ten year period Silfvast and Pettila (2003) reviewed hypothermic patients admitted to hospital in cardiac arrest and concluded that CPR performed over very prolonged periods for victims of cardiac arrest due to primary hypothermia was well tolerated. Wik and Kiil (2005) suggest that victims of cardiac arrest due to hypothermia should be seen as potentially resuscitatable with a prospect of recovery.
Mechanical CPR can be used as a bridge to other resuscitation therapy. In some cases this therapy may be rewarming, cardiopulmonary bypass or percutaneous coronary intervention. A small number of cases have been reported where LUCAS was used effectively while advanced resuscitation techniques were performed (Wik and Kiil 2005, Holmstrom et al 2005 and Larsen et al 2007). Without LUCAS or other such mechanical devices to provide an adequate systemic blood flow over a long time period and maintain life these interventions would not be possible.
Does LUCAS CPR improve survival rates?
Yannopoulos et al (2004) reported that the effects of inadequate chest recoil had considerable negative effects on cerebral and coronary perfusion. A number of studies have looked at active chest compression – decompression devices verses survival rates in adults. Lafuente et al (2004) conducted a literature review of a number of clinical trials comparing manual with active chest compression devices concluding that the use of active chest compression devices had no clear advantages over manual compressions. Their data collection and analysis was thorough with the author independently extracting data and contacting the original authors for further information which makes this paper credible. Rubertsson and Karlsten (2005) studied the efficacy of LUCAS during cardiopulmonary resuscitation in pigs and compared this to manual external compressions. Chest compressions with LUCAS resulted in higher brain blood flow and cardiac output however survival rate when compared with manual compressions was the same. Steen et al (2005) studied out of hospital cardiac arrest and while concluding there was no improvement in survival rate they highlighted some remarkable cases where LUCAS was successful. It should be noted that Steen et al (2005) were financially supported by a grant from the university where LUCAS was designed and the remarkable cases quoted may have been successful despite the intervention of a mechanical device. De Knock et al (2006) reported no difference in good neurological survival compared with standard chest compressions when data was analysed from ten hospital and seven prehospital cardiac arrests. Another study by Axelsson et al (2006) concluded that LUCAS did not improve out of hospital cardiac arrest survival rate. Current evidence is unable to support that LUCAS CPR improves either survival rate or neurological outcome and randomised control trials are required to study the potential benefits of mechanical chest compression devices.
Attitudes towards LUCAS
Attitudes by health care staff towards the use of mechanical devices are important as confidence in equipment can often dictate if a device is used in the emergency setting. De Knock et al (2006) observed that the incorporation of LUCAS into their advanced life support equipment was very well appreciated by both nursing and medical staff participating in resuscitation attempts. Halliwell (2004) in an evaluation of LUCAS use in Dorset Ambulance Service surveyed eighty six staff trained in the use of LUCAS with 100% of staff responding to the survey reporting confidence when using the device. This paper revealed that staff felt LUCAS was safe and easy to use in the ambulance with 96% of staff feeling the device was beneficial to the patient. This evidence is supported by anecdotic evidence from other users of the device.
Mechanical CPR discussion, limitations, implications & conclusions
The advantages of manual compressions are that they can be immediately performed by the rescuer, are adaptable to various field conditions and suitable for all patients regardless of size. Manual chest compressions can however be stressful, result in fatigue within a short time period (Hightower et al 1996) are difficult to perform during transport and performance amongst rescuers varies. Despite recent developments with the introduction of the LUCAS and other mechanical CPR devices into the clinical setting mechanical compression remains in the early days of development.
While there are worthwhile advantages a number of basic problems exist with the LUCAS device such as the availability of an adequate gas source, high noise levels and risk of combustion when used with oxygen. The need to develop equipment that performs effective CPR and ventilation to free the hands of the rescuer(s) is paramount. These devices must fit the following criteria; 1) easy to apply and operate, 2) quiet, 3) light weight, 4) portable to facilitate transport to the casualty 5) operate during patient transport 6) financially viable for mass deployment and, 7) deliver high quality compressions which meets latest guidance.
Increased cortical cerebral blood flow as reported by Rubertsson and Karlsten (2005) during LUCAS operation may result in an increase in patient level of consciousness bringing unknown and undesirable side effects such as patient awareness due to increased brain perfusion. There is a need to thoroughly research mechanical CPR devices using randomised controlled trials to provide an evidence base that will support or discourage clinical use. Until then mechanical devices should be used with caution by a single rescuer during patient transport, during special clinical circumstances or during prolonged CPR in both the hospital and out of hospital setting.
References.
Aston, A., McCluskey, A., Gwinnutt, A.L. and Keenan, A.M., 2002. Effect of Rescuer fatigue on performance of continuous external chest compressions over 3 min. Resuscitation, 55 (1), pp.151 – 155.
Aufderheide, T., Pirrallo, R., Yannopoulos, D., Klein, J., Von Briesen, C., Sparks, C., Deja, K., Kitscha, D., Provo. T. and Lurie, K., 2006. Incomplete chest wall decompression: A clinical evaluation of CPR performance by trained layperson and an assessment of alternative manual chest compression-decompression techniques. Resuscitation, 71 (3), pp. 341 – 351.
Axelsson, C., Nestin, J., Svensson, L. Asa, B. and Herlitz J., 2006. Clinical consequences of the introduction of mechanical chest compression in the EMS system for treatment of out of hospital cardiac arrest. A pilot study. Resuscitation, 71, pp.47 – 55.
Baubin, M., 1999. Increased injury of thoracic injuries with ACD-CPR. Resuscitation, 23, pp. 33 – 38.
Black, C.J., Busuttil, A. and Robertson, C., 2004. Chest wall injuries following cardiopulmonary resuscitation. Resuscitation, 63, pp. 339 – 343.
Control of Noise at work Regulations. No. 1643. 2005. [online] Available from: http://www.opsi..gov.uk [cited July 30th 2007].
Deakin, C.D., Paul, V., Fall, E., Petley, G.W. and Thompson, Fizz., 2007. Ambient oxygen concentrations resulting from use of the Lund University Cardiopulmonary resuscitation. Resuscitation, 74, pp.303 – 309.
De Knock, J., Martens, P., Muller, N., Van den Brande, F., 2006. The use of LUCAS for in and out of Hospital cardiac arrest. Resuscitation, 70 (2) pp. 305.
Englund, E. and Kongstad P.C. 2006. Active compression-decompression CPR necessitates follow-up post mortem. Resuscitation, 69 (1), pp. 161 -162.
Farmery, J.S. and Carter, M. 2007. Use of the Lund University Cardiopulmonary Assist System in the MD902: a fire safety assessment. Emergency Medical Journal, 24 (2), pp 110 -111.
Halliwell, D., 2004. Product evaluation in the Dorset Ambulance Service of the LUCAS chest compression/decompression device. Used as an alternative to manual chest compression, the device was evaluated in clinical use with adult patients in cardiac arrests. Resuscitation, 3, pp 10 – 11.
Hightower, D., Thomas, S.H., Stone, C.K., Dunn, K. and March, J.A., 1996. Decay in quality of closed-chest compressions over time. Resuscitation, 31 (3), pp. 86 – 87.
Hoke, R.S. and Chamberlain, D., 2004. Skeletal chest injuries secondary to cardiopulmonary resuscitation. Resuscitation, 63, pp. 237 – 338.
Holmstrom, P. Boyd, J., Sorsa, M. and Kuisma, M., 2005. A case of hypothermic cardiac arrest treated with an external chest compression device (LUCAS) during transport to rewarming. Resuscitation, 67, pp. 139 – 141.
Jolife, AB. 2005. LUCAS, External Cardiac Compressor, Instructions for use manual. Article no. 100081-00.
Jones, A.Y.M., 2004. Can cardiopulmonary resuscitation injure the back? Resuscitation. 61 (1), pp. 63 – 67.
Lafuente, C. and Melero-Bascones, M., 2004. Active chest compression-decompression for cardiopulmonary resuscitation. Cochrane Database of Systematic Reviews, Issue 4. Art. No. CD002751.
Larsen, A.I., Hjornevik A.S., Ellingsen. C.L. and Nilsen, D.W.T., 2007. Cardiac arrest with continuous mechanical chest compression during percutaneous coronary intervention. A report on the 1use of the LUCAS device. Resuscitation. In Press.
Lockey AS, Nolan JP., 2001. Cardiopulmonary resuscitation in adults (editorial). British Medical Journal. 323 (1), P.819 - 820.
LUCAS technical data sheet. [online] Available from http://www.lucascpr.com/ [cited July 30th 2007].
Lurie, K.G., Voelckel, W.G., Zielinski, T., McKnite, S., Lindstrom, P., Peterson, C., Wenzel, V., Linder, K., Samniah, N. And Benditt, D., 2001. Improving standard cardiopulmonary resuscitation with an Inspiratory impedance threshold valve in a porcine model of cardiac arrest. Anaesthesia and Analgesia, 93, pp.649 – 655.
Medical Devices Agency., 1995. Risk of fires when using oxygen in an oxygen enriched atmosphere . [online] Available from: http://www.mhra.gov.uk [cited August 10th 2007].
Moser, D.K. and Coleman, S., 1992. Recommendations for improving cardiopulmonary resuscitation skills retention. Heart lung. 41 (4), pp. 372 – 380.
Nolan JP, Deakin CD, Soar J, Bottiger BW, Smith G., 2005. European Resuscitation Council guidelines for resuscitation. Section 4, Adult advanced life support. Resuscitation. 67 (1), pp. 539 – 586.
Oberladstaetter D. Walker, R, Martin, F and Baubin M., 2006. Thorax injuries after LUCAS-CPR on female cadavers. Resuscitation, 70, (2), pp. 313.
Ochoa FJ, Gomara ER, Lisa V, Saralegui I., 1998. The effect of rescuer fatigue on the quality of chest compressions. Resuscitation, 37 (1), pp. 149 – 152.
Resuscitation Council (UK)., 2001. Guidance for safer handling during resuscitation in
hospitals.[online] Available from: http://www.resus.org [cited August 10th 2007].
Rubertsson, S., Grenvik, A., Zemgulis, V. and Wiklund, L., 1995. Systemic perfusion pressure and blood flows before and after administration of epinephrine during experimental CPR. Critical Care Medicine, 23, pp. 1984 – 1996.
Rubertsson, S. and Karlsten, R., 2005. Increased cortical cerebral blood flow with LUCAS; a new device for mechanical chest compressions compared to standard external chest compressions during experimental cardiopulmonary resuscitation. Resuscitation, 65, pp. 357 – 363.
Silfvast, T. and Pettila V., 2003. Outcome from severe accidental hypothermia in Southern Finland – a 10 year review. Resuscitation, 59, pp. 285 – 290.
Soar, J., Deekin, C.D., Nolan, J.P., Abbas, G., Alfonzo, A., Handley, A.J., Lockey, D., Perkins, G.D. and Thies, Karl., 2005. European resuscitation guidelines for resuscitation. Cardiac arrest in special circumstances. Resuscitation, 67S1, pp. 135 – 170.
Stapleton, E.R., 1991. Comparing CPR during ambulance transport. Manual vs. mechanical methods. Journal of Emergency Medicine, 16, pp. 63 – 68.
Steen, S., Sjoberg, T., Olsson, P. and Young, M., 2005. Treatment of out of hospital cardiac arrest with LUCAS, a new device for automatic mechanical compression and active decompression resuscitation. Resuscitation, 67, pp.25 – 30.
Sunde, K., Wik, L. and Steen, P.A., 1997. Quality of mechanical, manual standard and active compression-decompression CPR on the arrest site and during transport in a manikin model. Resuscitation, 34, pp. 235 – 242.
Valenzuela, T.D., Kern, K.B., Clarke, L.L., Berg, R.A., Berg, M.D., Berg, D.B., Hilwig, R.W., Otta, C.W., Newburn, D. and Ewy, G.A., 2005. Interruptions of chest compressions during emergency medical systems resuscitation. Circulation, 112, pp. 1259 – 1265.
Van Hoeyweghen RJ, Bossaert LL, Mullie A, Calle P, Martens P, Buylaert WA, Delooz H., 1993. Quality and efficiency of bystander CPR. Resuscitation, 26 (1), pp.47 -52.
Vatsgar, T., Ingebrigtsen, O., Fjose, L., Wikstrom, B., Nilsen, J. and Wil, L., 2005. Cardiac arrest and resuscitation with an automatic mechanical chest compression device (LUCAS) due to anaphylaxis of a woman receiving caesarean section because of pre-eclampsia. Resuscitation, 68, pp. 155 – 159.
Weil, M.H., Bisera, J., Trevina, R.P. and Rackow, E.C., 1985. Cardiac output and end-tidal carbon dioxide. Critical Care Medicine, 13, pp. 907 – 909.
Wik, L and Kiil, S., 2004. Use of automatic mechanical chest compression device (LUCAS) as a bridge to establishing cardiopulmonary bypass for a patient with Hypothermic cardiac arrest. Resuscitation, 66, pp. 391 – 394.
Woorhees, W.D., Babbs, C.F. and Tacker, W.A., 1980. Regional blood flow during cardiopulmonary resuscitation in dogs. Critical Care Medicine, 8, pp.134 – 136.
Yannopoulos, D., McKnite, S., Aufderheide, T.P., Sigurdsson, S., Pirrallo, R.G., Benditt, D. and Lurie, K.G., 2005. Effects of incomplete chest wall decompression during cardiopulmonary resuscitation on coronary and cerebral perfusion pressures in a porcine model of cardiac arrest. Resuscitation, 64, pp. 363 – 372.
Register
If you do not have access please register here to access our members section. If you have forgotten your password please click here to reset your password.
Contact Us
| Address | PO Box 1491 Dungannon BT71 5YF |
| Telephone: | 028 8774 6864 |
| Mobile: | 079 7662 1643 |
| Email: | info@survival-linx.com |